Safe GIST Surgery: Protocols for Better Outcomes
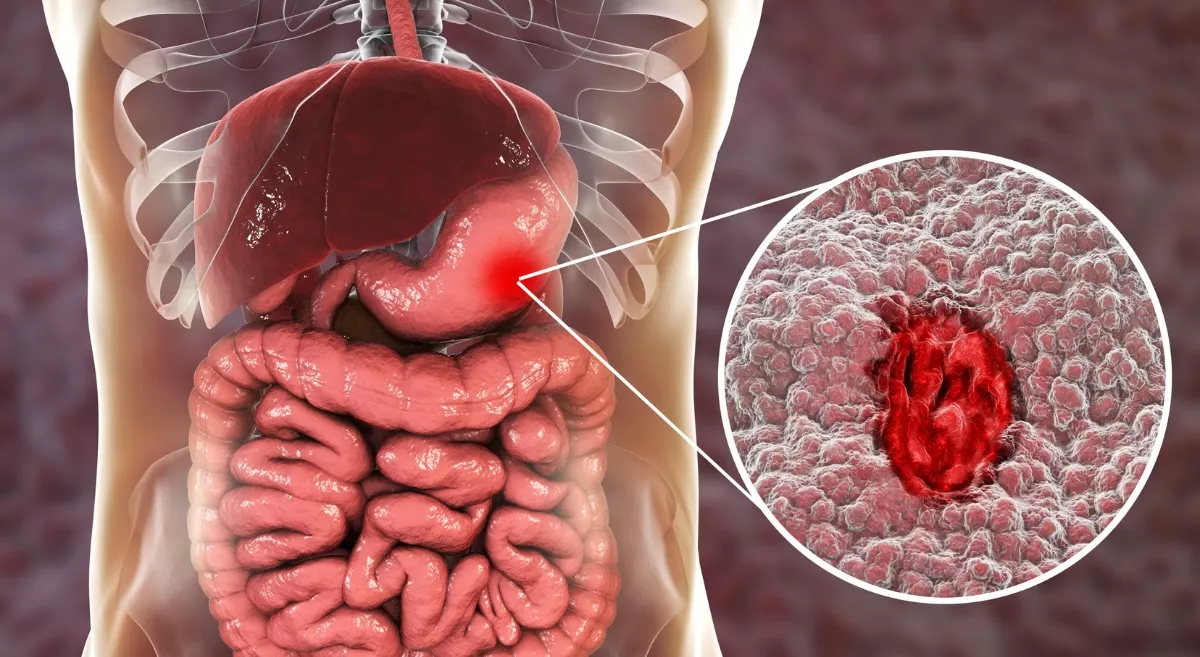
Have you or someone you know been diagnosed with a Gastrointestinal Stromal Tumour (GIST)? You may have a lot of questions, and that’s completely normal. GISTs are a rare type of cancer that begins in the walls of the digestive tract. They can appear anywhere from the oesophagus to the rectum, but most often, they are found in the stomach.
For many patients, surgery is the most effective treatment. But here’s something important to know: successful outcomes don’t just depend on removing the tumour. The real difference comes from the safety protocols and careful steps doctors follow before, during, and after surgery. These protocols are designed to keep you safe, minimize risks, and provide the best possible chance of long-term recovery.
In this blog, let’s explore the protocols that ensure safe GIST surgery and how your doctors work as a team to give you the best possible outcome.
The Power of a Multidisciplinary Team
Safe GIST treatment is never a one-person job. The first protocol doctors follow involves a multidisciplinary team.
A typical GIST team may include:
- Surgical Oncologist: A surgeon trained in cancer surgery who performs the actual GIST resection
- Medical Oncologist: Manages targeted drug therapy before or after surgery
- Radiologist: Uses CT scans and other imaging to locate the tumour and check for spread
- Pathologist: Examines removed tissue to confirm diagnosis and predict tumour behaviour
- Endoscopist: Helps detect or remove small tumours using minimally invasive procedures
This team-based approach ensures that every aspect, from diagnosis to surgery and recovery, is covered, giving patients the best chance of a safe and successful outcome.
Dr. Deep Goel explains, “The strength of a multidisciplinary approach lies in collaboration. When surgeons, oncologists, radiologists, and pathologists work together, the patient benefits from a 360-degree treatment plan.”
Precise Pre-Operative Planning
The journey to safe surgery begins long before the operating room. Careful preoperative optimisation reduces the risks of GIST surgery and ensures patients are fit for the procedure.
Accurate Diagnosis and Staging
- CT scans of the chest, abdomen, and pelvis are standard to check tumour size and spread
- Endoscopic ultrasound (EUS) helps measure tumour depth and assess high-risk features
Biopsy Considerations
Unlike other cancers, a biopsy is not always done for small, easily removable GISTs. This is because piercing the tumour capsule can cause cancer cells to spill into the abdomen, a complication known as peritoneal seeding.
- If a biopsy is required (for unresectable tumours or when drug therapy is planned first), it is performed very carefully with EUS-guided fine-needle aspiration.
A patient of Dr. Deep Goel shared, “After months of stomach discomfort and weight loss, I was diagnosed with a GIST. Meeting Dr. Goel changed everything. He took the time to explain what this rare tumour meant and why surgery was the right option. His detailed planning and emphasis on safety gave me the confidence to proceed. The operation was smooth, and I was back on my feet sooner than I imagined. I feel healthier now and deeply thankful for his guidance and expertise.”
Dr. Goel notes, “Pre-operative planning is about precision. A single misstep, like an unnecessary biopsy, can complicate surgery. That’s why detailed imaging and careful decision-making are key.”
The Cornerstone of Surgery: The “No-Touch” Technique
The most critical surgical rule in safe GIST surgery is the “no-touch” technique. GISTs are soft and have delicate capsules that can rupture easily, allowing cancer cells to spread. To avoid this:
- Gentle Handling: Surgeons avoid touching the tumour directly and instead handle the surrounding tissues
- En Bloc Resection: The tumour is removed in one piece, along with a margin of healthy tissue, to ensure no fragments are left behind
- No Routine Lymph Node Removal: Unlike many other GI cancers, GISTs rarely spread to lymph nodes, so lymph node dissection isn’t needed, reducing side effects
This careful handling helps in preventing GIST surgery complications and improves patient survival.
Choosing the Right Surgical Approach
The type of surgery depends on the tumour’s size, location, and involvement with nearby organs.
Minimally Invasive GIST Surgery
- Best for tumours smaller than 5 cm in favourable locations.
- Done using laparoscopy or robotic surgery.
- Benefits include smaller scars, reduced pain, a shorter hospital stay, and a quicker recovery.
Open Surgery (Laparotomy)
- Recommended for very large tumours or those in difficult locations.
- Sometimes requires the removal of part of the stomach or intestine if the tumour has grown into them.
Organ-Sparing Techniques
For tumours near sensitive areas like the gastroesophageal junction or duodenum, surgeons aim to remove the cancer while preserving as much of the organ as possible. This helps maintain digestive health and overall quality of life.
Dr. Goel emphasises, “Every GIST surgery is unique. The challenge is not just removing the tumour, but doing it in a way that preserves organ function and minimises long-term side effects.”
Another patient of Dr. Deep shared, “When I was told I had a GIST tumour in my stomach, my first thought was fear. Dr. Goel explained everything in simple terms, how the tumour would be removed, and what risks were involved. His confidence in using a minimally invasive approach reassured me. The surgery went smoothly, and to my surprise, I was able to walk the very next day. A year later, I’m healthy, active, and grateful for the safe hands I was in.”
The Role of Adjuvant and Neoadjuvant Therapy
Surgery is the primary treatment, but some patients benefit from drug therapy either before or after the operation.
- Neoadjuvant therapy (before surgery): Drugs like imatinib shrink large or complex tumours, making surgery safer and sometimes allowing minimally invasive techniques
- Adjuvant therapy (after surgery): Imatinib may be prescribed for months or years in high-risk patients to reduce recurrence
These treatments, guided by a medical oncologist, play a crucial role in ensuring optimal outcomes for GIST surgery.
Post-Operative Care
Surgery doesn’t end in the operating room. Safe GIST surgery protocols also include strict post-operative care and long-term monitoring.
Immediate Post-Surgery Protocols
- Infection prevention: Antibiotics and sterile wound care
- Pain management: Medications tailored for comfort and safety
- Early mobilisation: Patients are encouraged to walk early to prevent clots
- Nutritional support: Gradual reintroduction of fluids and soft foods
Long-Term Surveillance
- Regular imaging (CT or EUS): To detect any recurrence early
- Clinical follow-ups: Monitoring recovery and side effects of ongoing drug therapy
These steps help prevent complications from GIST surgery and ensure patient safety.
Why Surgeon Expertise Matters
The surgeon’s skill is one of the most significant factors in determining the success of GIST resection. An experienced GIST surgeon knows how to:
- Choose the safest surgical approach
- Prevent rupture during surgery
- Handle complex tumour locations
- Reduce long-term risks and improve the GIST surgery survival rate
When selecting a GIST surgeon, patients should seek specialists with extensive experience in gastrointestinal oncology surgeries.
How Patients Can Support Safer Outcomes
Doctors follow strict safety measures, but patients also play a crucial role in ensuring the safety of GIST surgery.
- Follow pre-surgery instructions, such as fasting or stopping blood-thinning medicines.
- Be honest about your medical history, including allergies and medications.
- Adopt healthy habits, such as quitting smoking, managing diabetes, and maintaining a balanced diet.
- Attend follow-up visits to catch any recurrence or side effects early.
Final Thoughts
GIST cancer surgery remains the most effective treatment for this rare tumour. What makes it truly safe and successful is the set of strict protocols doctors follow at every stage. From detailed pre-operative planning to the “no-touch” surgical technique and ongoing follow-up care, each step is designed to minimise risks.
With the expertise of skilled surgeons and modern medical support, patients can feel more confident about their treatment. Safe GIST surgery today means fewer complications, better recovery, and a brighter future.
FAQs on Safe GIST Surgery
1. What is the recovery time after GIST surgery?
Most patients recover within 4–6 weeks, with a quicker recovery time in minimally invasive surgery.
2. How long do patients stay in the hospital after GIST surgery?
Most patients stay 5–7 days after open surgery and 3–4 days after minimally invasive surgery.
3. Can GIST come back after surgery?
Yes, recurrence is possible, especially in high-risk tumours. This is why regular follow-up scans and, in some cases, additional drug therapy are essential after surgery.
4. Is minimally invasive GIST surgery safe?
Yes, for smaller tumours, it is considered a very safe and effective treatment. It reduces blood loss, hospital stay, and recovery time compared to open surgery, while still following all safety protocols.
5. How often should follow-up scans be done after GIST surgery?
Follow-ups are typically scheduled every 3–6 months for the first 3–5 years, then annually thereafter. The exact schedule depends on the patient’s risk profile.
Explore more blogs: GIST Cancer Surgery – Treatment, Recovery, Cost & Survival