What Can You Expect Before, During, and After Colon Cancer Surgery?
Colon cancer remains a significant global health concern, impacting millions of lives annually. According to the World Health Organisation (WHO), over 1.9 million new cases of colon cancer were reported globally in 2020. Additionally, nearly 0.9 million deaths were attributed to this disease within the same year.
Amidst this daunting landscape, colon cancer surgery stands as a cornerstone in the fight against this disease, offering hope and a path toward recovery for many.
Understanding what transpires before, during, and after colon cancer surgery is pivotal for patients and their families. This journey begins with a diagnosis, guiding individuals through crucial decision-making processes regarding treatment options, including surgery, chemotherapy, and radiation. The preparatory phase involves meticulous planning. Patients undergo thorough evaluations and lifestyle adjustments to ensure readiness for the surgical intervention.
During surgery, various approaches are employed to remove cancerous tissues—these range from traditional open procedures to minimally invasive and robotic-assisted techniques. Post-surgery, the road to recovery involves vigilant monitoring and rehabilitation. Long-term follow-ups are essential to ensure optimal healing and mitigate the risk of recurrence.
This blog delves into each phase of colon cancer surgery, offering insights into what patients can expect. Additionally, we explore the global landscape of this disease and the advancements reshaping treatment paradigms worldwide.
What Constitutes the Colon?
The colon, also known as the large intestine, is a crucial part of the digestive system. It’s a long, hollow tube that helps the body absorb water and nutrients from food and eliminate waste before it exits.
What defines Colon Cancer?
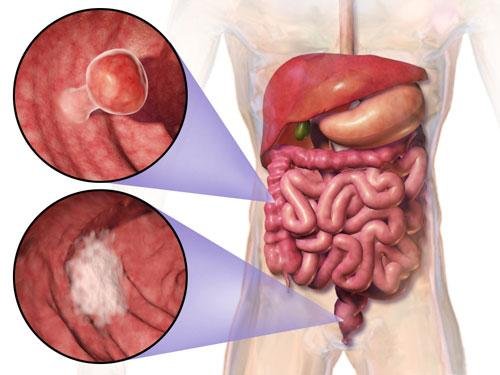
Colon cancer, also known as colorectal cancer, arises when abnormal cells within the colon or rectum undergo uncontrolled growth. These malignant cells can form tumours, potentially spreading to nearby tissues and organs.
How does Colon Cancer develop?
Colon cancer’s development primarily begins with genetic mutations in the cells lining the colon or rectum. These mutations, often unnoticed, instigate the formation of benign growths known as polyps on the colon’s inner wall. While not all polyps turn cancerous, certain types, particularly adenomatous polyps, can evolve into cancerous growths
Risk factors contribute significantly to this progression. A family history of colon cancer, advanced age, inflammatory bowel diseases like Crohn’s or ulcerative colitis, unhealthy diets rich in red or processed meats, sedentary lifestyles, and smoking can heighten the risk of these polyps transforming into cancer.
The unchecked growth of these abnormal cells leads to the formation of malignant tumours. Over time, these cancerous cells can invade surrounding tissues and, if not detected early and treated, may spread to distant body parts, a process known as metastasis.
Regular screenings, such as colonoscopies, play a pivotal role in identifying and removing polyps before they develop into cancer, highlighting the significance of early detection and intervention in managing colon cancer.
What Preparations and Expectations Precede Surgery?
Preparing for colon cancer surgery is a critical step that sets the stage for successful treatment and recovery. Here’s what patients can expect before going for surgery:
a) Diagnosis and Decision-Making
Upon diagnosis, patients often undergo a series of consultations to understand the severity and stage of their cancer. This phase involves discussions with healthcare providers to weigh various treatment options, including surgery, chemotherapy, radiation, or a combination thereof.
b) Preoperative Preparation
Before surgery, patients will receive comprehensive instructions for preparation. This might involve dietary changes, bowel preparation, and cessation of specific medications. Patients might also undergo preoperative tests to ensure they are fit for surgery, which include blood tests, imaging studies, and consultations with anesthesiologists.
c) Mental and Emotional Preparation
Preparing for surgery goes beyond physical readiness. Patients may experience emotional turbulence and anxiety. Engaging with support groups, counsellors, or trusted individuals can help patients cope with these emotions.
Dr. Deep Goel, a leading Gastrointestinal and Laparoscopic surgeon, explains, “We don’t just prepare patients physically for surgery, we prepare them emotionally. Addressing mental health is just as crucial as clinical readiness before any major procedure.”
What Happens During the Surgery?
Understanding what happens during colon cancer surgery can ease patient anxiety and clarify the treatment process. Here’s a look at the surgical phase:
a) Surgical Approaches
Colon cancer surgery encompasses various approaches, such as traditional open surgery, laparoscopic (minimally invasive) surgery, and robotic-assisted procedures. The specific method chosen depends on the tumour location, size, and the patient’s overall health.
b) Surgical Steps
During the surgery, the primary goal is to remove the cancerous tissue while preserving as much healthy tissue as possible. Surgeons might perform a resection (removal of the affected part of the colon) and possibly lymph node removal. The surgery’s duration varies based on complexity but typically lasts a few hours.
Dr. Deep Goel states, “With the evolution of technology, we now offer procedures that are less invasive, cause less pain, and enable quicker recovery while still ensuring complete cancer removal.”
What to Expect After Surgery?
Recovery after colon cancer surgery involves physical healing and emotional reassurance. Here’s what patients can expect post-surgery:
a) Immediate Postoperative Period
Following surgery, patients are closely monitored in the recovery room before being transferred to a hospital room. Pain management, intravenous fluids, and monitoring for potential complications are essential during this phase.
b) Hospital Stay and Rehabilitation
The length of the hospital stay varies depending on the extent of the surgery and the patient’s recovery progress. Patients gradually resume a liquid diet, advancing to solid foods under medical guidance. Physiotherapy and early mobility prevent complications like blood clots and promote recovery.
A patient of Dr. Deep shares, “After my laparoscopic colon cancer surgery, I was walking by the second day. The care team made me feel safe every step of the way. Dr. Goel’s confidence gave me the strength to stay positive during recovery.”
c) Long-Term Recovery and Follow-Up
As patients return home, they continue their recovery journey. This phase involves slowly regaining strength, managing potential side effects, and scheduling regular follow-up appointments with oncologists and surgeons. These visits include imaging tests and blood work to monitor for any signs of recurrence.
“Six months after my surgery, my scans showed no evidence of disease. I’ve returned to gardening and spending time with my grandchildren. The surgery gave me my life back,” shares a 63-year-old patient of Dr. Deep from Kenya.
What about the Global Perspective and Advancements?
Globally, colon cancer treatment has significantly evolved with the rise of advanced surgical techniques. Minimally invasive procedures, such as laparoscopic and robotic-assisted surgeries, have become increasingly common due to their precision and patient-friendly outcomes. These techniques offer smaller incisions, reduced blood loss, less postoperative pain, and faster recovery times compared to traditional open surgery. Leading cancer centres worldwide are adopting these innovations, improving overall survival rates and enhancing patients’ quality of life. Moreover, enhanced recovery protocols and real-time imaging have further optimised surgical planning and outcomes.
Conclusion
Colon cancer surgery is a significant step in a patient’s battle against this disease. Understanding the phases—preparation, the surge, and the postoperative journey—empowers individuals to navigate this challenging but crucial process effectively. As global statistics emphasise the prevalence of colon cancer, advancements in surgical techniques offer hope, better outcomes, and an improved quality of life for patients worldwide. Education, preparation, and a comprehensive support system ensure a smoother journey before, during, and after surgery.
FAQs
1. Will I need a colostomy bag after colon cancer surgery?
Not always. It depends on the tumor’s location. Many patients don’t need one, and if created, it may be temporary.
2. How soon can I return to work or normal activities?
Usually within 2–6 weeks, depending on the surgery type and your overall recovery.
3. Will my bowel habits change after surgery?
Yes, temporarily. Some patients may have lasting changes, but symptoms often improve with time and management.
4. Is it safe to travel or fly after surgery?
Yes, after 4–6 weeks if you’re stable. Always check with your doctor first.
5. Can colon cancer return after surgery?
Yes, which is why regular follow-ups with scans and blood tests are important for early detection.
Explore more blogs: Colon Cancer Surgery: What You Need to Know?